Maltreated Children and EMDR.
metanymous в Metapractice (оригинал в ЖЖ)
Моделируем EMDR, выпуск 21
| Сводная тема | |||||
| 25. Лево-правая экспрессия = EMDR (?) | metanymous | ||||
| Моделируем EMDR | |||||
| 22. EMDR Therapy Annotated Research Bibliography (2016) | metanymous | ||||
http://metapractice.livejournal.com/489916.html
Treating the effects of Trauma in It’s Infancy: Maltreated Children and EMDR.
http://insidethealcoholicbrain.com/2016/01/18/treating-the-effects-of-trauma-in-its-infancy-maltreated-children-and-emdr/
Neural processing of emotions in traumatized children treated with Eye Movement Desensitization and Reprocessing therapy: a hdEEG study. Eye Movement Desensitization and Reprocessing (EMDR) therapy has been proven efficacious in restoring affective regulation in post-traumatic stress disorder (PTSD) patients.
However, its effectiveness on emotion processing in children with complex trauma has yet to be explored. In this excellent study (1) high density electroencephalography (hdEEG) was used to investigate the effects of EMDR on brain responses to adults’ emotions on children with histories of early maltreatment.
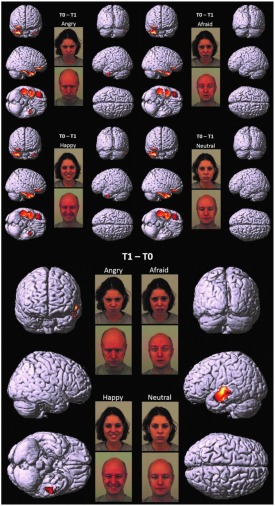
“Ten school-aged children were examined before (T0) and within one month after the conclusion of EMDR (T1). hdEEGs were recorded while children passively viewed angry, afraid, happy, and neutral faces. Clinical scales were administered at the same time. Correlation analyses were performed to detect brain regions whose activity was linked to children’s traumatic symptom-related and emotional-adaptive problem scores. In all four conditions, hdEEG showed similar significantly higher activity on the right medial prefrontal and fronto-temporal limbic regions at T0, shifting toward the left medial and superior temporal regions at T1. Moreover, significant correlations were found between clinical scales and the same regions whose activity significantly differed between pre- and post-treatment. These preliminary results demonstrate that, after EMDR, children suffering from complex trauma show increased activity in areas implicated in high-order cognitive processing when passively viewing pictures of emotional expressions. These changes are associated with the decrease of depressive and traumatic symptoms, and with the improvement of emotional-adaptive functioning over time.
Post-traumatic stress disorder (PTSD) describes discrete conditioned behavioral and biological responses to an experience involving actual or threatened death, serious injury, or sexual violence. The exposure must result from one or more of the following scenarios, in which the individual: (a) directly experiences the traumatic event; (b) witnesses the traumatic event in person; (c) learns that the traumatic event has occurred to a close family member or close friend (with the actual or threatened death being either violent or accidental); or (d) experiences first-hand repeated or extreme exposure to aversive details of the traumatic event (American Psychiatric Association, 2013).
Post-traumatic stress disorder, as diagnosis for adult onset trauma, is often applied to traumatized children as well. Nevertheless, a PTSD diagnosis fails to account for the complex symptomatology that emerges following early chronic interpersonal traumatization (such as psychological maltreatment, physical and sexual abuse, neglect, separation from caregivers, traumatic loss, and the witnessing of domestic violence). In the attempt to more clearly delineate childhood trauma impact, the diagnostic construct “complex trauma” has been proposed to describe the consequences of early children’s exposure to multiple and prolonged interpersonal traumatic events that occur primarily within the caregiving system (van der Kolk, 2005).
Early interpersonal traumatization exerts a deleterious impact on children’s abilities to recognize, express, and regulate emotional states. Several studies have found that maltreated children exhibit less accurate recognition of emotions in others than non-maltreated children, and have a selective attentional bias toward the detection of anger (Pine et al., 2005). Physically abused children display a boundary shift for perceptual categories of anger (Pollak and Kistler, 2002), require less visual information to detect angry facial expressions (Pollak and Sinha, 2002), and recognize cues related to aggression earlier (Pollak et al., 2000, 2009). These attentional biases have been explained as the effects of exposure to a physically abusive environment, where anger may be associated with the potential for physical threat or harm to the child (Pollak et al., 2000). Other studies have demonstrated that, relative to non-maltreated comparison groups, maltreated children show a faster and more accurate response to fearful (Masten et al., 2008) and sad facial expressions (Leist and Dadds, 2009), and are more likely to perceive neutral faces as angry or sad (Leist and Dadds, 2009). Compared to both physically abused and non-maltreated children, neglected children (who have received less support from adults in learning to decode emotional signs) appear to have more difficulties in discriminating emotional expressions (Pollak et al., 2000).
Neuroimaging research has extensively measured regional cerebral blood flow (rCBF) in adults (Francati et al., 2007) and children (Hart and Rubia, 2012) with PTSD, as compared to that of healthy controls. Investigations by positron emission tomography (PET) and single photon emission computed tomography (SPECT) have identified a hyper-reactivity of the amygdalae with acquisition of fear responses, and an impairment of the medial prefrontal cortex (mPFC) in properly regulating fear extinction, that could account for increased PTSD symptoms with traumatic reminders (Bremner, 2007; Looi et al., 2010).
With respect to the therapeutic approach, several studies have provided evidence for the clinical efficacy of Eye Movement Desensitization and Reprocessing (EMDR) therapy (Shapiro, 1989) in the treatment of PTSD (Shapiro, 2012). EMDR practice is guided by the adaptive information processing model (AIP model), (Shapiro, 2001) according to which a high level of disturbance related to traumatic experiences causes the information processing system to fail to properly process and store experience into the functional memory networks. The goal of EMDR is to access these dysfunctionally stored experiences and to transform them into adaptive ones, by stimulating the natural neural processes of memory consolidation (Shapiro, 2012). EMDR standardized protocol is structured in eight phases and requires the subject to focus on traumatic memories (target), while simultaneously being exposed to alternating bilateral stimulation (i.e., eye movements, tactile taps, or auditory tones)…
On the basis of such empirical evidence, EMDR has been recommended as a first-line trauma treatment in the international practice guidelines of several organizations, including the American Psychiatric Association (2004).
Attempts to explain the mechanisms of action involved in EMDR have documented that eye movements may enhance memory retrieval and attentional flexibility, reduce the vividness, emotionality, and completeness of unpleasant or traumatic memories, decrease psychophysiological arousal and increase parasympathetic activity in people with PTSD symptoms (see Shapiro, 2014).
Recent evidence of the effectiveness of eye movements is provided by the working memory theories of EMDR (Gunter and Bodner, 2008; Maxfield et al., 2008; van den Hout and Engelhard, 2012). Working memory research has found that performance is impaired when participants engage in two simultaneous tasks that compete for the same limited working memory resources (Baddeley, 2000). In line with this, several studies have found that eye movements reduce the ability to hold a visual image in conscious awareness, resulting in the degradation of vividness (for a systematic review, see Lee and Cuijpers, 2013).
Another model to account for the possible role of eye movements that has received some empirical support is the orienting response theory. Consistent with such theory, eye movements activate an “investigatory reflex” in which, at first, a state of heightened alertness occurs; then, a reflexive pause produces de-arousal, allowing cognitive processes to become more flexible and efficient (Kuiken et al., 2001; Lee and Cuijpers, 2013).
Over the last few years, neuroimaging studies have been used to investigate the neurobiological substrate of EMDR in clinical practice (Pagani et al., 2013; Pagani and Cavallo, 2014). SPECT studies have documented significant changes in CBF patterns after EMDR (Lansing et al., 2005; Pagani et al., 2007), reflecting the recovered inhibitory role of the prefrontal cortex (PFC) in reducing amygdala hyperactivation in response to pathological stimuli that recall the traumatic event. Structural Magnetic Resonance Imaging (MRI) investigations have also provided some evidence that EMDR in PTSD may be associated with changes in limbic and paralimbic gray matter density, and with improvement of symptoms (Nardo et al., 2010; Bossini et al., 2012).
…bilateral stimulation might be associated with: a reduced attention to novel stimuli and a diminished arousal level after therapy (Lamprecht et al., 2004); a depotentiation of fear memory synapses in the amygdala (Harper et al., 2009); and a decrease of the interhemispheric EEG coherence, which may foster the consolidation of traumatic memories, thereby reducing traumatic memory intrusions (Propper and Christman, 2008). Recently, the possibility to monitor by EEG, in real time, the relative neurobiological modifications occurring upon EMDR has been proposed (Pagani et al., 2011, 2012). The comparison between the EEGs of patients during the first and last session has showed, during the latter, a significant deactivation of the orbitofrontal and subcortical limbic structures, as well as a greater activation in the left temporo-occipital cortex (Pagani et al., 2012), suggesting that traumatic events had been processed at cognitive level following therapy…
Discussion
Early maltreatment alters the trajectories of brain development, decreasing the functionality of cerebral regions related to emotion processing (Curtis and Cicchetti, 2011;Hart and Rubia, 2012)…
Before EMDR (T0 vs. T1), significant cortical activations were found in inferior/medial PFC as well as TP and ITG, with a prevalent lateralization in the right hemisphere. After EMDR therapy (T1 vs. T0), we found a reduced activity in these cerebral regions and a significant increase of cortical activation in lMTG and lSTG.
The significantly higher activation found in children at T0 as compared to T1 in the right regions of inferior/medial PFC – OFC and IFG, respectively, – may reflect the dysfunctional ability in these children in decoding affective cues and regulating inner responses to adults’ emotions…
These findings are coherent with those of previous studies, which indicate the impairment of mPFC in regulating the response of the limbic system (including the amygdala and the related nuclei and circuitry) to stimuli that resemble traumatic events (Bremner, 2007; Looi et al., 2010; Pagani et al., 2011,2012). It has been suggested that early and prolonged stress may result in more prefrontal cortical catecholamine concentration (especially norepinephrine and dopamine) than is functionally necessary to cope with the stressors. Extreme levels of dopamine, in particular, may impair frontal inhibition of the limbic system, exaggerating attention and vigilance toward cues that are experimented as potentially traumatic (De Bellis et al., 2011). Prefrontal activation is implicated in the introspective evaluation of self-generated material (Ramnani and Owen, 2004) and in the decoding of the emotional value of incoming information (Steele and Lawrie, 2004). Moreover, PFC is involved in autobiographical memory retrieval (Tulving et al., 1994) and in the suppression of unwanted memories during autobiographical recall (Anderson et al., 2004). All these functions seem to be exaggerated in patients before EMDR therapy, since the self-referential emotional contents cause larger activation in rPFC than in normal individuals or in patients after having processed the traumatic event (Pagani et al., 2012).
At T0 as compared to T1, higher response to all adult emotions was also found in rTP, a paralimbic area which, in conjunction with inferior frontal lobe structures, is activated during autobiographical memory retrieval (Engdahl et al., 2010). Previous studies indicate that activation in rTP increases when subjects attend more “socially relevant” dimensions of a visual display, such as emotions, therefore modulating the amygdala response to threat/fearful stimuli (Olson et al., 2013). Moreover, rTP (together with rmPFC) is activated when inferring the thoughts and the feelings of other people is used to guide personal social behaviors (Olson et al., 2013).
Lastly, significantly higher activity was found at T0 as compared to T1 in ITG. This region also plays a key role in memory recall; moreover, in conjunction with the adjacent fusiform gyrus, it is implicated in face perception and recognition, receiving greater contribution from the amygdala especially during the processing of fearful expressions (Schupp et al., 2004).
Before EMDR, cerebral responses in children did not vary according to the specific valence of the presented emotions. These results are coherent with scientific literature on complex trauma, according to which children who are exposed to early and prolonged traumatic events often experience intense negative affects (such as rage, betrayal, fear, resignation, defeat, and shame), associated with a persistent sensibility to negative emotions. The aim is to prevent potentially traumatic experiences.
Such enhanced sensitivity causes a long-term emotional dysregulation, characterized by over- or/and under reactivity to emotional minor stimuli that would have no significant impact on non-maltreated children (van der Kolk, 2007). In line with this, research has shown that maltreated children have poor discriminatory abilities for different facial emotions and misinterpret all emotional faces (including neutral and happy ones) as being threatening or as a mask for more malevolent emotions (Pollak et al., 2000; Leist and Dadds, 2009; van Harmelen et al., 2013).
Further relevant neurobiological results which emerged in our study were the differences shown between the cortical activation at T1 as compared to T0…
In this comparison, we found a reduced activity after EMDR intervention in the right regions of inferior/medial PFC, as well as rTP and ITG, and a significant increase of cortical activation at T1 in lMTG and lSTG.
These temporal areas play a key role in social cognition, since they encode and retrieve autobiographical memory, process concepts with social–emotional content, and associate highly perceptual and emotional information to form a personal semantic store (Olson et al., 2013). The MTG modulates emotional processes, such as sensitivity to threatening cues, anxiety and mood disorders (Davidson, 2004). It has been suggested that early and prolonged traumatic experiences may impair the functioning of this region, encompassing the amygdala and the hippocampus (Maheu et al., 2010).
Even though from different perspectives, current theories on the mechanisms of action involved in EMDR provide possible explanations of the neurobiological changes we observed over time in children.
According to the AIP model (Shapiro, 2001), EMDR allows to access traumatic memories which are dysfunctionally stored, transforming them into adaptive ones, by stimulating the natural neural processes of memory consolidation (Shapiro, 2012). Once the memory retention of the traumatic event can move from an implicit subcortical status to an explicit cortical one, the traumatic memories and their related emotions may be elaborated at higher cognitive level. Coherently with the results of previous researches (Pagani et al., 2012), our study seems to indicate that, after EMDR, children use high-order cognitive resources while processing emotion expressions.
The working memory theories of EMDR may provide a further significant contribution to the explanation of the results of our study. Working memory allows the individuals to access memories, retrieve related material, compare this to what they are currently perceiving, integrate new material with old material, and form new understandings to guide future behaviors (Baddeley, 2000). Research in EMDR domain has consistently found that the vividness and emotionality of memory is reduced when individuals are simultaneously engaged in performing eye movements and focusing on a traumatic image, since both tasks make demands on the same limited working memory resources (Gunter and Bodner, 2008; Maxfield et al., 2008; van den Hout and Engelhard, 2012). As a result, the target memory is perceived as less distressing and is more likely to be processed from an observational or detached perspective (Maxfield et al., 2008). In our study, such “distancing” effect (Lee et al., 2006) may have allowed children to regulate inner responses to adults’ emotions through the use of higher cognitive processes.
It is important to notice that the increase in efficiency of cognitive processes is a key point of the orienting response theory of EMDR (Armstrong and Vaughan, 1996; Kuiken et al., 2001; Lee and Cuijpers, 2013). Consistent with such theory, eye movements may induce attentional flexibility, thereby facilitating the re-elaboration of the subjective representation of traumatic experiences.
As at T0, activations at T1 in cognitively relevant areas did not vary according to the specific valence of the emotional stimuli. This result shows that EMDR did not affect the children’s capacity to discriminate different emotional expressions: it rather appears that EMDR may have contributed in globally restoring the processing of emotional cues (regardless of their type), resulting in all faces being processed and contextualized in semantic memory in the same way.
Conclusion
To our knowledge, this is the first study that has investigated the effects of EMDR on brain responses to adults’ emotions on children with complex trauma. Our preliminary findings have demonstrated that after EMDR, early maltreated children show increased activity in areas implicated in high-order cognitive processing when passively viewing pictures of emotional expressions. These changes are associated with the decrease of depressive and traumatic symptoms, and with the improvement of emotional-adaptive functioning over time. These results may have relevant implications in clinical practice, suggesting the importance of focusing interventions with traumatized children on cognitive processing of emotions.
References
An Insight Into How Trauma May Be "Healed"In "EMDR"
The Effectiveness of EMDR Therapy on the Emotion Regulation and Emotion Recognition of Addicted IndividualsIn "addiction"
How the Brain "reacts" to EMDR?In "neural correlates of EMDR"
Categories: childhood maltreatment, Complex PTSD, dopamine, EMDR, PTSD
Tagged as: childhood maltreatment, Complex PTSD, dopamine, EMDR, PTSD
Post navigation
2 комментария
сначала старые сначала новые
http://www.myreviews.it/140188_emdr-la-terapia-che-salva-le-vittime-dei-traumi/